As global and U.S. agencies officially declared the end of the pandemic phase of COVID-19 on May 5, 2023, many expressed deep relief. The United Nations described the pandemic as a “once-in-a-lifetime” event, and many, believing another pandemic not plausible within their lifetimes, have been sliding back from healthy habits. Over 10% fewer people stated they wash their hands “all or most of the time” compared to the beginning of the pandemic, according to a cross-pandemic study conducted by the United Kingdom’s Food Standard Agency.
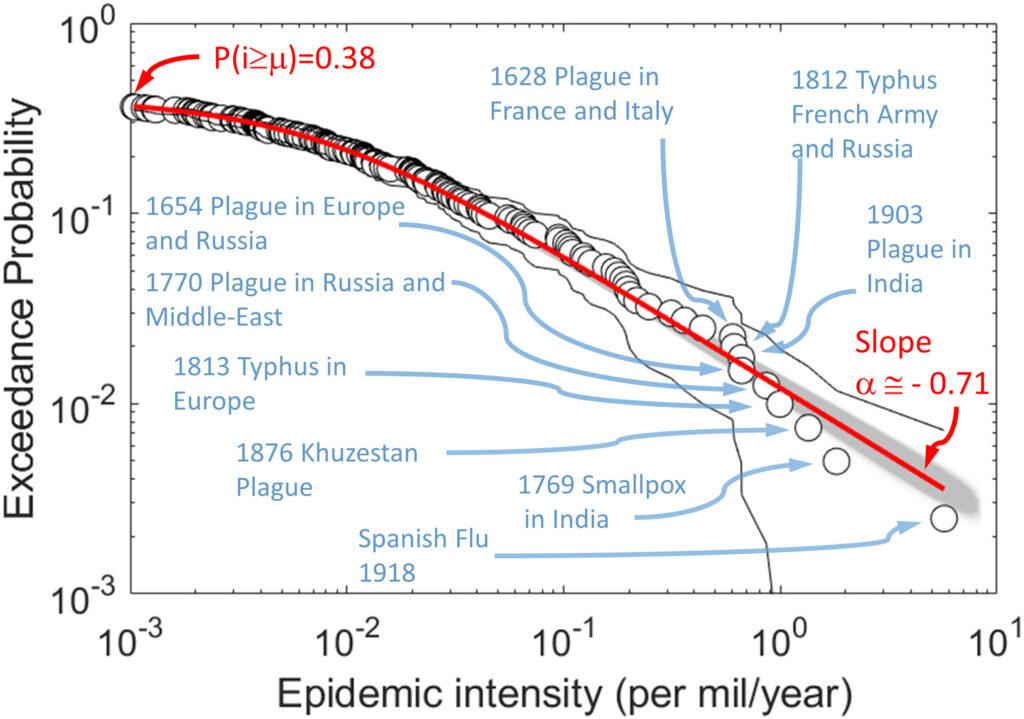
To some extent, those that are moving away from strict pandemic guidelines have a point. Historically, a major pandemic is uncommon, happening every 100 years or so: the Cholera pandemic in the 1820s and the Spanish flu pandemic in the 1920s preceded the COVID-19 pandemic in the 2020s.
Nevertheless, we’ve recently seen a drastic rise in epidemics, such as the pre-COVID SARS epidemic from 2002-2004 and the ongoing HIV-AIDS epidemic that started in 1981. Major disease outbreaks have consistently been a problem, especially in modern times. If anything, the time between them seems to be shortening.
In November, China experienced the outbreak of a new strain of pneumonia that raised concerns from the World Health Organization (WHO). COVID isn’t over yet either — a new variant, called JN.1, has spread across the world, doubling its cases over the recent holiday season.
The rise in novel diseases has been troubling. Indeed, a study published in the Proceedings of the National Academy of Sciences compared empirical pandemic data and current epidemiological factors. It found that the probability of an extreme epidemic will triple in the coming decades, due to the increased connectivity of society, among other factors.
Individuals and governments need to prepare for future pandemics by improving the response system to prevent the spread of dangerous pandemic misinformation and focus on improving our organizational and infrastructural capabilities.
Throughout COVID-19, misinformation about the pandemic was extremely widespread and had harmful impacts. In a survey asking adults eight false statements about COVID, such as “the government is exaggerating the number of COVID-19 deaths” and “you can get COVID-19 from the vaccine,” over 80% of those surveyed believed at least one false statement was true.
Misinformation regarding a potentially fatal pandemic can have devastating results. In the first three months of 2020, the WHO found COVID-related misinformation led to the hospitalization of 6,000 people and the deaths of 800 more.
Furthermore, in a study analyzing over 80 million Twitter posts, researchers concluded that casual misinformation contributed to an over 150% increase in pandemic anxiety across all demographics, with the effect on minorities being most pronounced.
When people refuse to wear masks, stay at home or get vaccinated due to misinformation, their choices can seriously hinder society’s recovery.
What should we do? Although efforts are currently being made, such as social media companies saying that they’ll tighten moderation on misinformation, they are not enough due to lack of enforcement. These companies should actively implement such moderation to combat misformation through flagging “misleading content” or altogether removing substantially harmful content. In addition to these efforts, people can actively listen to and correct misinformation.
Next, we need to improve our emergency pandemic preparedness. Having a plan to combat the pandemic is the most important thing society can do, which can involve taking what we know about our COVID-19 response and constructing a list for improvement. For instance, the government’s recent step of creating the Office of Pandemic Preparedness and Response Policy (OPPR) was beneficial, but more effort and specialization should be put into the OPPR to facilitate its growth.
The Center for Disease Control, for instance, started as a small organization dedicated to combating malaria, but later became a large, governmental organization that helps with public health issues nationwide. Organizations develop and grow, so taking a powerful, small step now can lead to a much more solidified pandemic response system in the future.
We should also construct the infrastructure necessary to manufacture and distribute pandemic testing, vaccines and other health products. Crucially, barriers to COVID testing were a major factor that exacerbated the pandemic. We could spend more resources on maintaining a healthy supply chain for distribution, or creating a more streamlined manufacturing capability.
Increasing availability of testing and vaccines, especially in rural areas, drastically reduced the spread of COVID-19. During the Omicron wave, increased testing in nursing facilities reduced the number of deaths by 26%, according to the National Institute of Health.Although the next pandemic may seem like something far off in the future, it’s actually much more likely than we think. Starting efforts now to combat misinformation and increase our preparedness would be extremely beneficial to future responses. To prevent another 7-million death tragedy like COVID-19, we need to redouble efforts now.