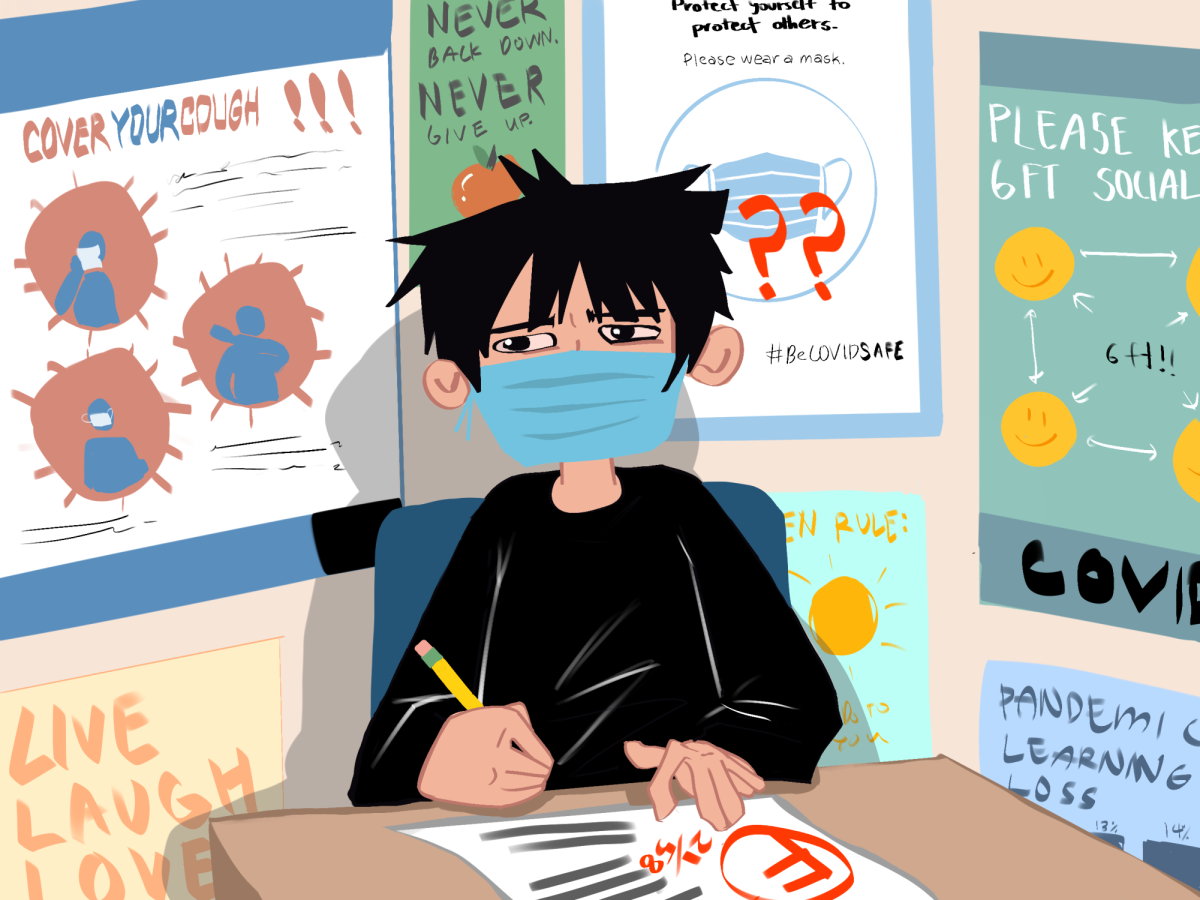
Two years ago, high school volunteers were scurrying around the spacious dining chapel at the Villa of Saratoga Assisted Living Facility to serve dinner for the elderly residents. These days, the room is set up into three stations: registration, vaccination and observation.
There, on Jan. 25, five nurses from the Santa Clara County Public Health Department gave the second dose of the Pfizer-BioNTech vaccine to the residents at the Villa, completing their COVID-19 vaccination.
Santa Clara County (SCC) is in Phase 1A and partial Tier 1 of Phase 1B, meaning all healthcare personnel and long-term care facility (LTCF) residents, as well as county residents age 65 or 75 — depending on the local system — and older, are eligible to be vaccinated.
As of today, 55,889 people in the county have received their second dose, while 3.0 percent of people statewide have had the same. Although the parties involved find that the vaccine distribution policies are far from perfect, with eligibility being clouded by confusions, scandals and vague guidelines, progress is being made toward improving the system.
“It's a matter of who's aggressive”
Ricaredo Concepcion, activities director at the Villa, said the facility’s 120 residents all received the first dose on Jan. 4 without objections; the staff members got their first dose at Santa Clara County Fairgrounds in late December.
“I know there are people who don’t believe in the vaccine, but fortunately within our residents and employees there's no problem,” Concepcion said.
In order to get the residents vaccinated, the infection control officer for the Villa had to apply to the county’s public health department.
The county’s public health department website has a dashboard to track the cases at long-term care facilities, which serve elderly individuals with medical conditions — a population at great risk of COVID-19 and is recommended to be offered the first supply of the vaccines, according to the CDC. However, not every long-term care facility on the dashboard has gotten vaccinations.
“It's a matter of who's aggressive,” Concepcion said. “Every [long-term care facility] has its name on the county dashboard, but there’s limited manpower, so you must be aggressive enough to call the county.”
Chateau Cupertino, an independent retirement community with almost 200 residents, has been attempting unsuccessfully to facilitate a vaccine clinic since November.
In a public comment submitted to the county’s Board of Supervisors, Camille Miller, activities director at Chateau Cupertino, wrote that her facility was told by the CDC, the state and the county that the residents must wait because they are not considered a long-term care facility.
However, with residents requiring assistance ranging from medication management to full 24-hour medical care, Miller believed that Chateau Cupertino residents deserved to be vaccinated and inquired about what was being done to resolve the situation.
“Cases for both residents and staff are rising daily, more so since the beginning of 2021,” Miller wrote. “When can we have a clinic for our residents?”
She has reached out to several other Independent Living Communities in the area, and they have not received clear answers either.
“It has been extremely difficult and frustrating for our seniors to have had to wait months for any information,” Miller said in an interview with The Falcon. “We should have been contacted by Santa Clara County to rectify our seniors being left behind.”
While Miller’s situation remains unresolved, another group that was initially left out by the distribution plan has since then gained a spot.
Class of 2006 alumna Katie Reed, a hospital manager at the Reed Animal Hospital, said that she received the good news on Jan. 8 that veterinarians and their staff were added to Phase 1A.
This change came because many veterinarians have written petitions to express their concerns about operating without being vaccinated, Reed said.
Vaccinating healthcare and education workers
Many local healthcare professionals have received COVID-19 vaccines, one of whom is Iris Li, a pediatrician who works at Los Gatos Pediatrics.
Li said she believes that the current way of distribution — in which only big hospitals can administer vaccines — will be too slow once more people become eligible. To speed up the process, she hopes that small clinics would be able to vaccinate people as well.
But the challenge is that many small clinics, like hers, do not have the -70 degree Celsius freezer that is necessary for storing the Pfizer-BioNTech vaccine. She said that to facilitate efficient distribution of vaccines beyond the initial phases, the authorities should equip small clinics with the necessary freezers.
But even the current way of distribution from big hospitals comes with its own problems, as seen in a recent scandal involving Los Gatos Union School District and San Jose’s Good Samaritan Hospital.
On Jan. 21, LGUSD superintendent Paul Johnson informed his staff that they could skip the line and receive COVID-19 vaccines early by registering as healthcare personnel because education workers are not yet eligible in the county. The maneuver was encouraged by Gary Purushotham, the chief operating officer for Good Samaritan.
As a result, Good Samaritan has been suspended from receiving vaccine doses from the county until it can provide a concrete plan to assure that it will follow guidelines on vaccine eligibility.
Antonio Castelan, media contact for Good Samaritan, said that the hospital has submitted a plan to the county.
“While vaccine storage limitations and fluctuating availability have been a challenge, we want to reassure our community that we have had only positive intentions throughout the vaccination process,” Castelan said in a statement to The Falcon. “We regret the mistake we made.”
Alexis Friedman, co-director and teacher at the Saratoga Parent Nursery School (SPNS), said that skipping the line is unethical even though she believes educators should be high on the priority list.
None of the three teachers at SPNS has been vaccinated, Friedman said. She is happy to see that educators are high on the priority list for California, but she expects to face challenges.
“I'm concerned that there won't be enough vaccines,” Friedman said. “Plus, we don't have a ‘badge’ that the elementary, middle and high school teachers have, and I haven't seen the state's plan on how to verify that someone is a teacher or caregiver.”
Friedman stresses the importance of vaccinating preschool teachers because online education is the most difficult for younger children.
“There's a 'window' of opportunity for tremendous learning before the age of five,” she said. “Children who miss this window to socialize will most likely have a harder time adapting to the elementary classroom, so it's important for early childhood educators to be vaccinated because in-person learning is crucial.”
Evolving plans targeting distribution
On Feb. 9, Levi’s Stadium opened as a mass vaccination site and administered 500 doses of coronavirus vaccines. County officials expect that the number of doses will rise to 5,000 per day by the following week and eventually to 15,000 per day, making it the largest vaccination site in California.
In the county’s Board of Supervisors meeting on Jan. 26, the testing and vaccine officer Marty Fenstersheib, M.D., said he believes that the county has done a good job with distributions given its limited resources.
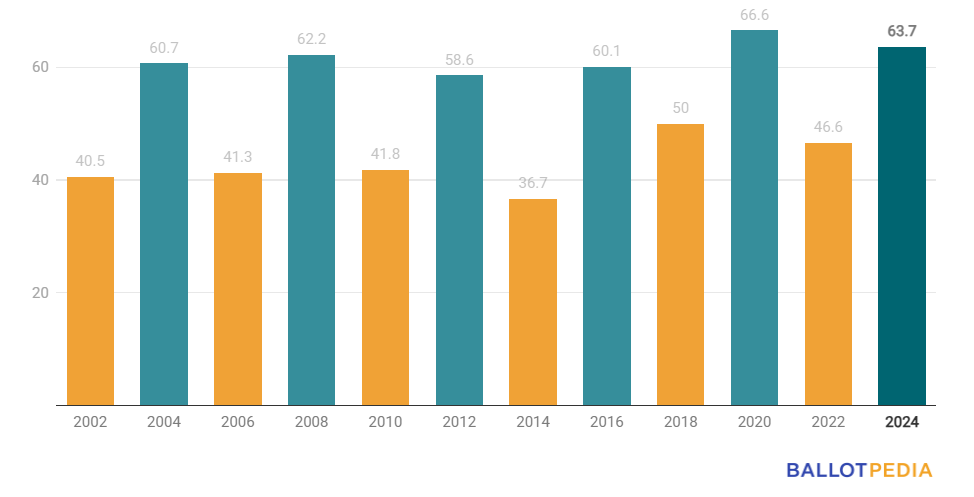
“If you add up all the first and second doses, you'll find that about 67 percent of all of the vaccines that we have received are in people's arms,” he said. “I think we are actually doing quite well with the limiting factor being vaccine availability.”
In an interview with The Falcon, Congresswoman Anna Eshoo, who represents the 18th District and chairs the House Health Subcommittee, said that the new administration is already increasing the supply in two ways. The first is sending more vaccines to states each week.
“As of [the week of Feb. 1], the Biden-Harris administration is sending out 10.5 million doses per week nationwide,” Eshoo said. “This is a 22 percent increase in delivered doses since the new administration took office.”
The federal government is also giving states estimates of the number of doses each state will receive three weeks in advance so that states can plan accordingly, she said.
The second part of the plan is to increase the country’s overall vaccine supply. The federal government already purchased 200 million doses each of the Pfizer and Moderna vaccines and plans to buy 100 million more doses of each, Eshoo said. Additionally, Johnson & Johnson has just applied for an Emergency Use Authorization for their single dose COVID-19 vaccine.
These actions are all part of the $1.9 trillion American Rescue Plan, which proposes to invest $20 billion in the vaccination program.
“Right now, I’m working to pass a law to provide $20 billion through the House Health Subcommittee,” Eshoo said. “The Biden-Harris administration has pledged 100 million shots in 100 days, and it is on track to meet this important goal.”
Although the numbers of vaccines allocated and administered are looking good, the county itself is seeing recent changes in state guidelines that leaves many things up in the air.
County executive officer Dr. Jeffrey Smith said in the Jan. 26 meeting that California announced a series of changes that day, including implementing standardized eligibility across all 58 counties and piloting a website called MyTurn to facilitate vaccination.
The most significant change, however, is that vaccine allocations will be shifting from the counties to two third-party administrators, Blue Shield of California and Kaiser Permanente, which will allocate vaccines directly to providers in order to maximize distribution efficiency.
The details and specific impacts of this change are currently unknown, he said.
“But we're all hopeful that the seriousness with which the Biden-Harris administration takes COVID-19 will translate to significant vigor in tackling this pandemic,” Smith said.